- Home
- Orthopedics
- Hardest Day After Knee Replacement: Pain Timeline, UK Tips, and Recovery Plan

Hardest Day After Knee Replacement: Pain Timeline, UK Tips, and Recovery Plan
You brace for agony right after surgery, then feel oddly okay for a while. And then, out of nowhere, day two smacks you. If you’re wondering which day is the hardest after a knee replacement and how to handle it without losing your mind, you’re in the right place. I live in London, I’ve seen this up close with friends and family, and I’ll give you a straight, practical plan that works in the UK system in 2025.
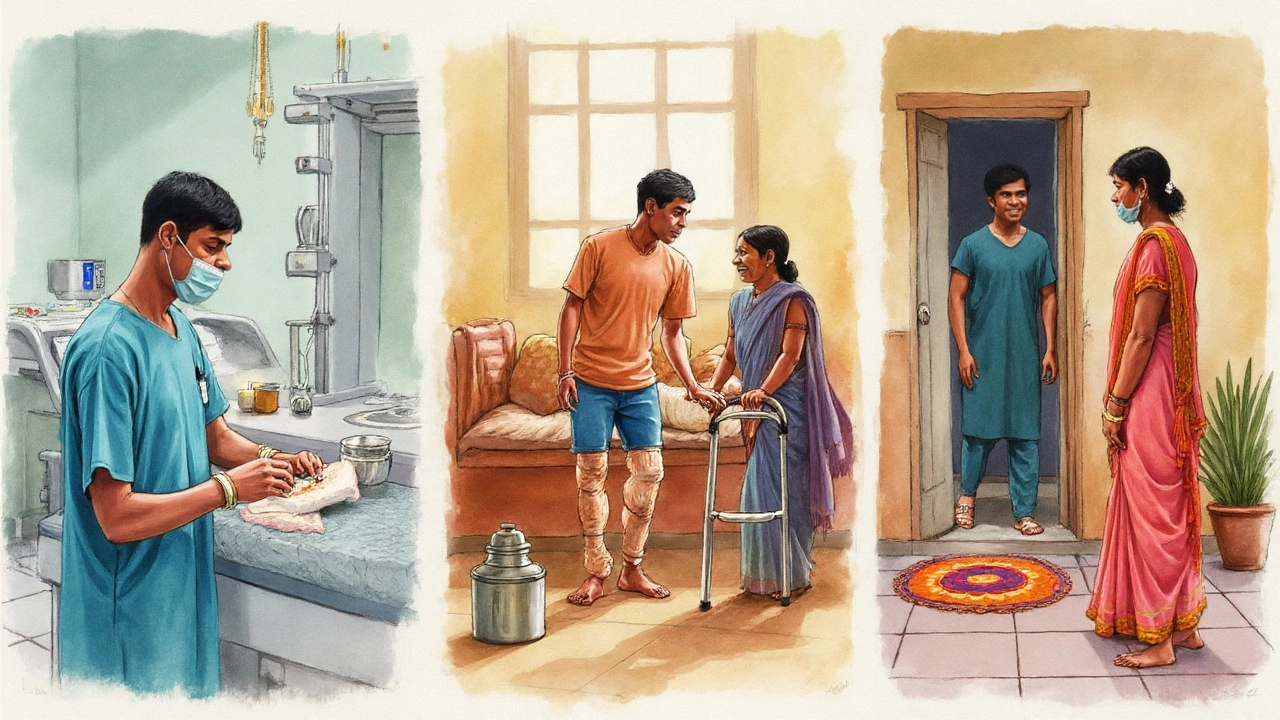
hardest day after knee replacement
TL;DR
- Most people hit the wall between 36-72 hours after surgery (day 2 to early day 3) as the nerve block wears off and swelling peaks.
- The fix isn’t one thing; it’s a stack: scheduled pain meds, ice, high elevation (“toes above nose”), gentle movement, and sleep tactics.
- Expect sleep to be rough for 1-2 weeks; it gets better faster if you protect knee extension and keep the swelling down.
- Red flags you shouldn’t ignore: chest pain/shortness of breath, calf pain with heat, fever over 38°C, or wound leakage that’s getting worse.
- By the end of week 1, many reach 70-90° bend; by week 2, 90°+ is common. Your timeline may differ, and that’s normal.
What day is the hardest, and why does it hit then?
Short answer: for most patients, the toughest stretch is day 2 to early day 3. Day 0 and day 1 are often cushioned by a spinal anaesthetic and a nerve block. When that wears off (usually 12-36 hours after surgery), the joint wakes up, the pain signals flood in, and your leg starts to balloon. That’s the double whammy: the pain comes online just as swelling reaches its early peak.
What’s happening under the skin? Your knee has been resurfaced. Tissues are inflamed, and fluid rushes in. The capsule around the joint is tight, so pressure builds, especially when you let the leg hang down. That pressure makes bending feel brutal. It’s not you being weak; it’s mechanics.
In the UK, same-day or next-day discharge is routine now, so a lot of people hit day 2-3 at home. That can feel scary. It’s expected. The goal is to blunt that spike and stop swelling becoming your boss for the next two weeks.
| Time after surgery | Typical pain | Swelling | Why this happens | What helps most |
|---|---|---|---|---|
| 0-12 hours (Day 0) | Low-moderate | Low-moderate | Spinal/nerve block working, IV meds on board | Ice, start ankle pumps, regular meds as ordered |
| 12-36 hours (Late Day 1) | Rising | Rising | Blocks wearing off; you start moving more | Keep meds scheduled, ice, elevate high |
| 36-72 hours (Day 2-3) | Peak | Peak | Inflammation and fluid peak; sleep debt kicks in | Strict med timing, 20-min ice cycles, frequent short walks, elevation |
| Day 4-7 | Trending down | High but improving | Body starts clearing fluid; you move better | Build routine: meds, ice, extension stretch, heel slides |
| Week 2 | Moderate | Moderate | Tissue healing; strength waking up | Progress exercises; longer walks; sleep improves |
Evidence check: The Royal College of Anaesthetists notes single-shot adductor canal blocks often wear off within 12-24 hours; add a spinal and you can feel protected into day 1. The American Academy of Orthopaedic Surgeons (2023 CPG) backs “multimodal analgesia” (paracetamol plus an anti-inflammatory, with opioids only as needed) to reduce pain and cut opioid use. A Cochrane review found cold therapy can modestly reduce pain and swelling in the first 48 hours-so keep the ice handy. NHS/NICE pathways also stress early movement, VTE prevention, and wound vigilance.
A simple day-by-day plan for the first two weeks
You don’t need a perfect plan. You need a repeatable one. Here’s a simple routine that fits how pain and swelling behave. Use your surgical team’s instructions first; slot this in where it matches.
Daily rhythm (Days 0-7)
- Wake and dose on time. Don’t “wait for pain.” Keep paracetamol regular if approved for you. If you were given an anti-inflammatory (e.g., ibuprofen or naproxen) and it’s safe for you, pair it as prescribed with food. Opioids (like codeine or tramadol) only when needed and as directed. Set phone alarms every 6-8 hours-night too for the first 2-3 nights.
- Ice in cycles. 20 minutes on, 20-30 off, repeat 4-6 times a day. Wrap the cold pack in cloth; never on bare skin. Ice after exercises and before bed.
- Elevate properly. “Toes above nose” if you can, or at least hip level. Lie on your back with your heel supported so the knee can straighten. This drains fluid fast and protects extension.
- Move little and often. Every hour you’re awake: ankle pumps, 10-20 reps. Do a 2-5 minute walk around the room or hallway every 1-2 hours. Short and frequent beats one big slog.
- Protect extension. Two or three times a day, prop your heel so the knee hangs straight for 5-10 minutes. No pillow under the knee. This prevents a flexion contracture (the enemy of a smooth gait).
- Bend safely. Heel slides: on your back, slide heel toward your bottom as far as comfort allows, then straighten. 10 reps, 3-4 times daily. Stop if you see a big jump in swelling later.
- Eat, drink, and… go. Aim for protein with each meal, fibre, and fluids. If you’re on opioids, start a bowel plan day 0-stool softener plus a gentle stimulant (e.g., lactulose and senna) as advised by your team.
- Sleep in shifts. Naps are fine. At night, back-sleep with a pillow under the heel/calf, not under the knee. Side-sleep only if your team says it’s safe and use a pillow between knees.
Core exercises (Days 0-7) - light, frequent, pain-aware:
- Quad sets: press the back of your knee down, hold 5 seconds, 10 reps, 3-4 times daily.
- Ankle pumps and circles: 10-20 reps hourly while awake.
- Glute squeezes: 10 reps, 3-4 times daily.
- Heel slides: 10 reps, 3-4 times daily.
- Straight leg raises: only when you can lift without the knee buckling; start with 5 reps, build to 10.
Building from Day 8 to Day 14
- Walks: add a few minutes each day if swelling stays stable. Indoors to outdoors, flat surfaces first.
- Stationary bike: if cleared, no resistance, 5-10 minutes. Rock back-and-forth until you get a full turn.
- Stairs: up with the good, down with the operated leg first, handrail and stick as needed.
- Strength: short-arc quads (roll under knee), sit-to-stands from a higher chair, 2-3 sets of 5-10.
- Range goals: many reach 0-10° from straight and 90° bend by the end of week 2. Don’t force through sharp pain; coax it with heat before and ice after.
Medication rhythm that tends to work (confirm with your team)
- Paracetamol on schedule (e.g., every 6-8 hours) if you’re allowed it.
- Anti-inflammatory (if safe for you) with food and any stomach protection you were given.
- Opioid only when needed, lowest dose, shortest time. Add or start your bowel plan the same day.
- Blood thinner (as prescribed-aspirin, rivaroxaban, apixaban, etc.) and compression if told to use it. Keep walking bits hourly while awake.
Note: NHS trusts differ on details, but the principles line up across NICE guidance and UK orthopaedic pathways-regular non-opioid meds first, move early, protect extension, and stay ahead of swelling.
Pain, swelling, and sleep: the tools that actually help
You don’t need to be tough; you need to be consistent. Stack small wins. Here are the tools that move the needle the most on the worst days.
1) Timing is pain control
- Set alarms for meds and for icing. Pain is easier to prevent than to chase.
- If your pain is >7/10 even with meds, first check timing. Are you late on a dose? Is there room for the anti-inflammatory? Then add ice and elevation for 20-30 minutes. If it still stays >7, ring your surgical team or NHS 111 for advice.
2) Ice and height beat heat (early on)
- The first 72 hours are an ice-and-elevate sport. Keep the foot high, aim for the heel to be the highest point when resting.
- Think of swelling as thick treacle in the joint. Elevation drains it. Every hour your leg spends hanging down in a chair is like pouring more treacle in.
3) Move a little right now; move a lot later
- On peak days, break activity into tiny chunks. Two minutes of walking every hour still adds up. Joints love motion; tissues hate overload.
- Protect extension daily; flexion can come a touch slower without penalty. Getting the knee fully straight is the sneaky key to a normal gait.
4) Sleep: aim for total hours, not perfect nights
- Expect broken nights for 7-14 days. Naps count. A dark, cool room, a light snack, meds on board before bed, and a 20-minute ice session can turn down the volume.
- If your mind is racing, set a 10-minute timer and do box breathing (inhale 4, hold 4, exhale 4, hold 4). It’s simple, and it works.
5) Food, fluid, and bathroom strategy
- Protein with each meal speeds healing (eggs, Greek yogurt, lean chicken, lentils). Add vitamin C foods (berries, peppers) for collagen support.
- Constipation prevention starts day 0 if you’re on opioids. Don’t wait. Water, fibre, stool softener, a short walk after meals.
6) The psychology of the dip
- Day 2-3 can feel like you made a mistake. You didn’t. Expect the wobble, plan the response, and tell your support person what to do before it hits.
- Write your 3-sentence plan on a note: “If pain spikes, check med time, ice, elevate. If pain stays >7 for 2 hours: call the team. Keep doing ankle pumps.”
Caregiver quick sheet
- Guard the schedule: meds on time, water bottle full, food within reach.
- Set up an “ice station” and swap packs before they warm up.
- Check the dressing: dry and intact is good. Spreading redness, increasing drainage, or a bad smell-report it.
- Walk with them every 1-2 hours, even just to the kitchen and back.
FAQ and red flags: when to push, when to pause
You’ll have a few big questions during those rough first days. Here are clear answers and what to do next.
Is it normal that day 2 hurts more than day 1? Yes. As nerve blocks fade and you’re moving more, the knee often feels much worse. This is expected. Stick to the routine. Most people feel a noticeable drop in pain by day 4-5 if they control swelling.
How much should I bend in the first week? Comfortably as you can. Many people get 70-90° by the end of week 1. Don’t force it through sharp pain; use heat before, ice after, and coax the bend with heel slides. Extension (getting the knee flat) is the bigger early priority.
Should I be worried if I can’t sleep? Broken sleep is common for 1-2 weeks. Focus on total hours in 24 hours. Stack naps, keep caffeine earlier in the day, ice before bed, and set a loose wind-down routine. It gets better as swelling drops.
What pain score is too high? If you’re sitting at >7/10 for more than two hours after taking medicines on time, add ice and elevation and call your hospital team or NHS 111. If pain is sudden, severe, with a “pop,” or the leg won’t take weight, seek urgent care.
How do I know if swelling is normal? Big swelling is normal early on. It should start trending down after day 3-5. If it’s getting steadily worse, the calf is hot and tender, or the skin is getting very tight and shiny, that’s a flag. Combine that with shortness of breath or chest pain, and call emergency services immediately.
What about the dressing and showering? Most modern dressings are shower-proof after 48 hours if your team says it’s okay. Keep it dry otherwise. If the dressing is soaked through, leaking, or smells bad, that needs a call. Avoid soaking the wound (baths/pools) until you’re cleared.
When can I drive? For the right knee, usually when you can do an emergency stop safely and you’re off opioids-often around 4-6 weeks, but it varies. Left knee in an automatic can be sooner. Check with your surgeon and insurer.
What if I feel behind on range of motion? First, lower swelling: stricter elevation and icing can unlock bend. Add more frequent gentle heel slides and short bike “rocking.” If you’re below 90° by week 4, talk to your physio or surgeon about options. Plenty of people catch up with consistent work.
What if I have diabetes or I’m older? Healing and swelling can take longer, and infection risk is higher. Keep blood sugars tight, watch the wound daily, and pace yourself. The plan still works-expect a slower but steady curve.
Do partial and total knee replacements differ here? Partials often have a slightly easier pain curve and faster early bending, but day 2-3 can still be the bump. The same tools apply.
Red flags to act on now
- Chest pain, shortness of breath, coughing blood-call emergency services.
- Calf pain with heat/redness, one leg far more swollen than the other-urgent call to your team or NHS 111.
- Fever over 38°C with chills, worsening wound redness, pus-like drainage-contact your surgical unit.
- Numb foot, blue toes, or you suddenly can’t move the foot-urgent care now.
Troubleshooting by scenario
- Pain spikes every evening: You may be doing too much late in the day. Bring a walk or exercise set to the morning, add a mid-afternoon ice/elevation block, and take nighttime meds on time.
- Knee won’t straighten: Prop heel for 5-10 minutes, 3-5 times daily; add gentle quad sets. Avoid pillows under the knee.
- Knee won’t bend: Warm compress or shower, then heel slides and a few minutes on the bike rocking back and forth, then ice. Don’t force past sharp pain.
- Constipation: Start or increase stool softener as advised, drink water, and do short walks after meals. If no movement by day 3, call for advice.
- Opioid side effects: If you’re drowsy or nauseated, see if you can lean more on paracetamol and an anti-inflammatory (if safe), and take the smallest opioid dose needed. Ask your team about anti-nausea meds if necessary.
What to expect next
- By day 4-5: pain curve starts dropping if you’ve kept meds on schedule, iced, and elevated.
- By day 7-10: walking feels smoother; swelling still there but manageable.
- By week 2: 90°+ bend is common; stairs feel less scary.
- By weeks 4-6: many are driving (if cleared), doing longer walks, and trimming pain meds to basics.
Why you can trust this plan: It mirrors UK postoperative pathways (NHS/NICE), uses Royal College of Anaesthetists guidance on nerve block timing, AAOS-backed multimodal pain control, and the best available evidence on cryotherapy. It also matches what I’ve personally seen sitting with friends as they hit the day‑2 wall: when they stacked meds, ice, height, and frequent little walks, the rough patch passed faster.
This isn’t medical advice for your specific case. Your surgeon’s plan wins if there’s a clash. But if you wanted one clear answer-what’s the hardest day and how do I get through it-now you’ve got both. Day 2-3 is tough. You’re tougher, with a plan.

Arnav Singh
I am a health expert with a focus on medicine-related topics in India. My work involves researching and writing articles that aim to inform and educate readers about health and wellness practices. I enjoy exploring the intersections of traditional and modern medicine and how they impact healthcare in the Indian context. Writing for various health magazines and platforms allows me to share my insights with a wider audience.
About
Medical Resource Center India is a comprehensive online platform dedicated to providing reliable health information and medical resources in India. Explore a wide range of articles, tips, and advice on medicine, healthcare services, and wellness. Stay informed about the latest developments in Indian medicine and access valuable insights into maintaining a healthy lifestyle. Discover expert guidance and health solutions tailored for every Indian citizen. Your go-to destination for authoritative medical knowledge in India.








