- Home
- Weight Loss
- Eligibility Criteria for Weight Loss Medication in 2025

Eligibility Criteria for Weight Loss Medication in 2025
Weight Loss Medication Eligibility Checker
Enter your details and click "Check My Eligibility" to see if you qualify for weight loss medication.
Key Takeaways
- In the UK, you usually need a BMI≥30kg/m², or ≥27kg/m² with a weight‑related health condition, to be considered for prescription weight‑loss drugs.
- Doctors will ask you to have tried at least 3months of diet, exercise, and behaviour change before prescribing.
- Common approved medicines include semaglutide, liraglutide, orlistat, phentermine‑topiramate and naltrexone‑bupropion, each with its own BMI cut‑offs and side‑effect profile.
- Age (18‑65years is typical), pregnancy, certain heart conditions, and a history of pancreatitis are frequent contraindications.
- Discuss insurance coverage or NHS eligibility early, because cost can vary widely between private and public routes.
When you hear the term weight loss medication is a prescription drug designed to support weight reduction in people for whom lifestyle changes alone aren’t enough, you probably wonder whether you qualify. The answer hinges on a mix of measurable numbers, medical history, and proven attempts at lifestyle modification. This guide walks you through the exact criteria clinicians use in 2025, what makes each drug different, and how to position yourself for a successful prescription.
Who Can Be Considered for Medication?
In the UK, the National Institute for Health and Care Excellence (NICE) outlines clear thresholds. You’ll generally be eligible if you meet one of the following:
- Your body‑mass index (BMI) is 30kg/m² or higher.
- Your BMI is between 27kg/m² and 29.9kg/m² and you have at least one obesity‑related comorbidity such as type2 diabetes, hypertension, or obstructive sleep apnoea.
These numbers come from extensive research showing that the health benefits of medication-lower blood pressure, improved glycaemic control, reduced risk of heart disease-are most evident above these cut‑offs.
Key Medical Thresholds Explained
Let’s break down the main metrics doctors look at.
- Body‑mass index (BMI) is a simple calculation: weight (kg) ÷ height (m)². A BMI of 30kg/m² is the clinical definition of obesity.
- Type2 diabetes is a chronic condition where the body can’t use insulin effectively, often linked to excess weight.
- Hypertension (high blood pressure) raises the risk of heart attack and stroke, and weight loss can dramatically lower those numbers.
- Other qualifying conditions include dyslipidaemia, non‑alcoholic fatty liver disease (NAFLD), and obstructive sleep apnoea.
If you have any of these, they act as a green light for clinicians to consider medication once lifestyle attempts have been documented.
What Lifestyle Steps Must You Show First?
Prescription isn’t a shortcut. Doctors want proof you’ve tried the basics:
- At least three months of a structured lifestyle modification programme, which includes a calorie‑controlled diet and a minimum of 150 minutes of moderate‑intensity activity per week.
- Documented attempts-whether through a diet‑tracker app, a referral to a dietitian, or a weight‑loss group log.
- A clear statement that despite these efforts, your weight has plateaued or continued to rise.
These records help the clinician gauge whether medication will add real value or if more intensive behavioural therapy is still the first line.
Age, Pregnancy, and Other Contra‑indications
Most UK guidelines set the eligible age range between 18 and 65years, mainly because safety data beyond this window are limited. Additionally, the following situations typically rule out prescription:
- Current pregnancy or planning to become pregnant-weight‑loss drugs can affect fetal development.
- History of pancreatitis (especially relevant for GLP‑1 agonists like semaglutide).
- Severe cardiovascular disease, unless a specialist approves the specific drug.
- Personal or family history of medullary thyroid carcinoma (a rare concern for some GLP‑1 drugs).
Always disclose your full medical history; a thorough review can surface hidden blockers or alternative pathways.
Overview of Approved Medications (2025)
Below is a snapshot of the most commonly prescribed weight‑loss medicines in the UK, their mechanisms, and the BMI thresholds they require.
| Drug | Mechanism | Approved BMI | Typical Dose | Common Side Effects |
|---|---|---|---|---|
| Semaglutide (Wegovy) | GLP‑1 receptor agonist - reduces appetite & slows gastric emptying | ≥30kg/m² or ≥27kg/m² with comorbidity | 0.5mg weekly, titrated to 2.4mg weekly | Nausea, diarrhea, constipation |
| Liraglutide (Saxenda) | GLP‑1 agonist - similar appetite‑suppressing effect | ≥30kg/m² or ≥27kg/m² with comorbidity | Initial 0.6mg daily, up to 3.0mg daily | Nausea, vomiting, headache |
| Orlistat (Xenical) | Lipase inhibitor - blocks absorption of ~30% of dietary fat | ≥30kg/m² | 120mg three times daily with meals | Steatorrhea, oily spotting, abdominal cramps |
| Phentermine‑Topiramate (Qsymia) | Appetite suppressant (phentermine) + neuro‑modulator (topiramate) | ≥30kg/m² | Starting 3.75mg/20mg daily, titrated to 15mg/100mg | Dry mouth, insomnia, paraesthesia |
| Naltrexone‑Bupropion (Contrave) | Modulates appetite & reward pathways | ≥30kg/m² | Start 8mg/90mg daily, increase to 32mg/360mg | Nausea, constipation, increased blood pressure |
Each drug has a slightly different weight loss medication qualification profile. For example, GLP‑1 agents (semaglutide, liraglutide) are favored if you also have type2 diabetes because they improve glucose control simultaneously.
How to Talk to Your Doctor About Medication
Approach the conversation as a partnership, not a demand. Here’s a quick cheat‑sheet:
- Bring a written log of your diet, exercise, and any weight‑loss programmes you’ve tried.
- List any comorbid conditions-especially hypertension, type2 diabetes, or sleep apnoea.
- Ask about the specific drug’s BMI cut‑off, dosing schedule, and monitoring plan.
- Clarify whether the prescription would be covered by the NHS or if you’d need a private prescription.
- Discuss follow‑up frequency-most clinicians require visits every 3‑4months to assess efficacy and side‑effects.
Being transparent about your goals and concerns builds trust and improves the odds of a tailored treatment plan.
Insurance, NHS Funding, and Cost Considerations
In England, the NHS will fund weight‑loss medication only when the clinical criteria are met and lifestyle interventions have been documented. Private insurance may cover the drugs, but you’ll likely face an out‑of‑pocket cost ranging from £150 to £300 per month, depending on the medication.
If you’re uninsured or the NHS declines coverage, consider these options:
- Clinical trials-universities often recruit participants for new GLP‑1 agents.
- Prescription assistance programmes offered by pharmaceutical companies.
- Switching to a lower‑cost option like orlistat, which is available over the counter.
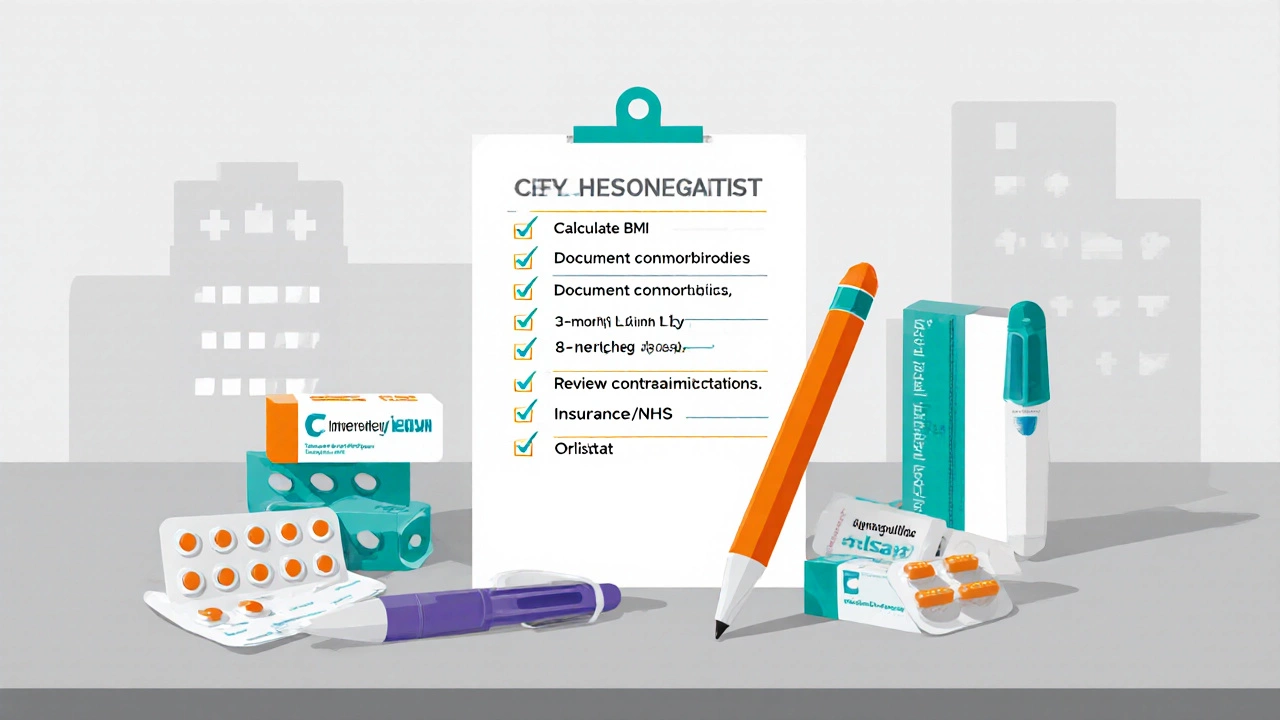
Checklist Before Your Next Appointment
- Calculate your current BMI and write it down.
- Gather medical records showing any comorbidities.
- Prepare a 3‑month log of diet & exercise attempts.
- List any contraindications (pregnancy plans, pancreatitis history, etc.).
- Research the medication you’re interested in and note its approved BMI threshold.
- Check NHS eligibility guidelines or private insurance coverage.
Frequently Asked Questions
Do I need a formal diagnosis of obesity to get a prescription?
Yes. Clinicians rely on a documented BMI of 30kg/m² or higher, or 27‑29.9kg/m² with a related health condition, as the baseline for prescribing.
Can I try a weight‑loss drug without trying diet and exercise first?
No. UK guidelines require documented lifestyle attempts for at least three months before medication is considered.
What if my BMI is 28 but I have type2 diabetes?
You meet the “BMI≥27 with comorbidity” rule, so you’re eligible for most GLP‑1 agents, provided you’ve tried lifestyle changes.
Are there any long‑term safety concerns?
GLP‑1 drugs have extensive 5‑year data showing good safety, but they’re not recommended for people with a history of pancreatitis or medullary thyroid carcinoma.
How often will my doctor monitor my progress?
Typically every 3‑4months for the first year, checking weight loss, blood pressure, glucose levels, and any side effects.

Arnav Singh
I am a health expert with a focus on medicine-related topics in India. My work involves researching and writing articles that aim to inform and educate readers about health and wellness practices. I enjoy exploring the intersections of traditional and modern medicine and how they impact healthcare in the Indian context. Writing for various health magazines and platforms allows me to share my insights with a wider audience.
Popular Articles
About
Medical Resource Center India is a comprehensive online platform dedicated to providing reliable health information and medical resources in India. Explore a wide range of articles, tips, and advice on medicine, healthcare services, and wellness. Stay informed about the latest developments in Indian medicine and access valuable insights into maintaining a healthy lifestyle. Discover expert guidance and health solutions tailored for every Indian citizen. Your go-to destination for authoritative medical knowledge in India.

