Stage 4 Cancer Survival: Facts, Options, and Hope
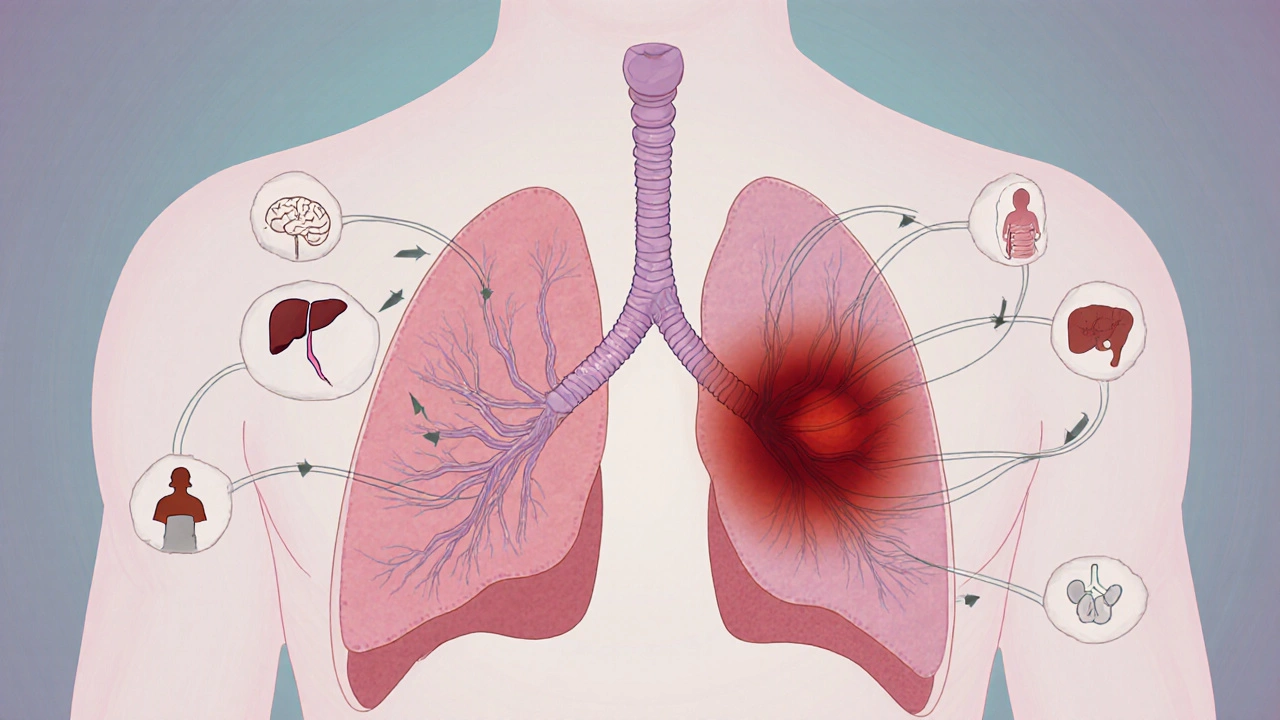
When working with stage 4 cancer survival, the outlook for living longer after an advanced cancer diagnosis. Also known as late‑stage cancer prognosis, it helps patients and families plan the next steps. This concept is tightly linked to stage 4 cancer, cancer that has spread beyond its original site and to the range of cancer treatment, therapies aimed at controlling growth and easing symptoms that can influence survival chances.
One key attribute of survival is the survival rate, which measures the percentage of people alive after a set period, usually five years. In stage 4 cases the rate varies by tumor type, genetics, and how quickly treatment starts. For example, targeted drugs can push the 5‑year rate from under 5 % to around 15 % in certain lung cancers. Knowing the exact numbers lets patients weigh benefits against side effects.
Another important concept is the idea of a terminal diagnosis, a medical opinion that the disease is unlikely to be cured. While many think terminal automatically means death within months, modern therapies often extend life months or years, blurring the line between “terminal” and “treatable”. Understanding this nuance can keep hope alive and guide decisions about palliative care.
What Influences Stage 4 Survival?
Three main factors shape outcomes: (1) the biology of the tumor – aggressive subtypes drop survival, while slower‑growing ones improve it; (2) the availability of advanced treatments – immunotherapy, precision medicine, and clinical trials add years; and (3) the patient’s overall health – nutrition, exercise, and mental support boost tolerance to intensive regimens. Each factor connects back to the central idea of survival, showing why a personalized plan matters.
Patients often ask whether “survival” means a full cure. The answer is no; survival describes staying alive, not being cancer‑free. However, many survivors achieve long‑term remission, meaning the disease stays under control for years. This distinction matters when families discuss goals, insurance coverage, and quality‑of‑life choices.
Palliative care plays a critical role even when the disease is advanced. It focuses on symptom relief, pain management, and emotional support, which can indirectly improve survival by keeping patients strong enough for further therapy. Integrating palliative specialists early often leads to better overall outcomes and reduces hospital admissions.
Clinical trials are another avenue that can shift the survival curve. Enrolling in a trial gives access to cutting‑edge drugs that aren’t yet widely available. Studies show that participants in oncology trials sometimes live longer than those receiving standard care, especially when the trial targets a specific genetic mutation.
Lifestyle choices remain powerful, even at stage 4. Regular, low‑impact exercise helps maintain muscle mass and circulation, while a balanced diet rich in protein and antioxidants supports immune function. Stress‑reduction techniques such as mindfulness or guided breathing can lower cortisol levels, which some research links to slower tumor progression.
Decision‑making in late‑stage cancer is a team effort. Oncologists, surgeons, palliative experts, and caregivers must align on realistic goals, balancing treatment intensity with quality of life. Clear communication about expected benefits, possible side effects, and the patient’s personal wishes makes the journey less overwhelming.
Below you’ll find a curated set of articles that break down stage differences, explain treatment options, and share real‑world tips for coping with a late‑stage diagnosis. Whether you’re looking for a quick overview or in‑depth guidance, the collection offers practical insight to help you navigate the tough road ahead.