Immunotherapy: A Practical Overview
When talking about immunotherapy, a treatment approach that harnesses the body’s own immune system to target disease. Also known as immune‑based therapy, it’s changing the way doctors tackle cancer, a group of diseases characterized by uncontrolled cell growth. The core idea is simple: boost or direct immune cells so they can recognize and destroy harmful cells. That basic principle opens the door to several distinct methods, each with its own set of tools and outcomes.
Key Players and How They Fit Together
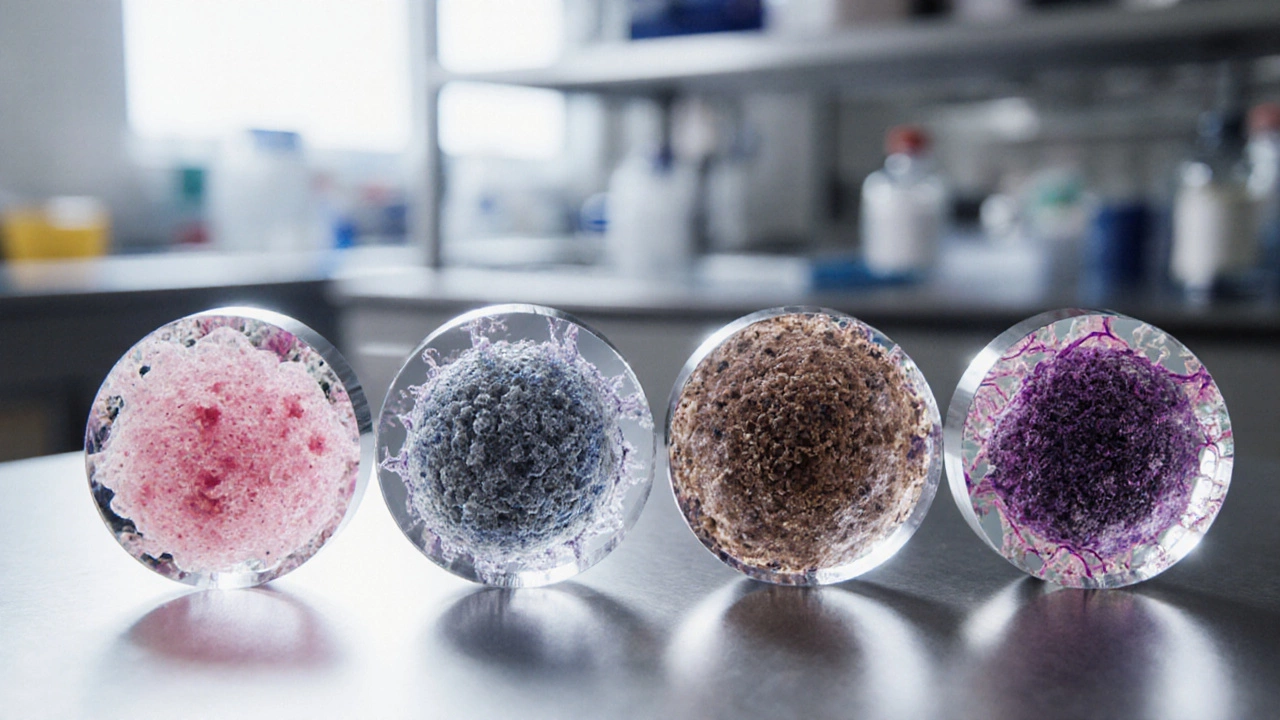
One of the most talked‑about methods is checkpoint inhibitors, drugs that block proteins that keep immune cells from attacking tumors. By releasing these “brakes,” checkpoint inhibitors let T‑cells go after cancer cells more aggressively, which often translates into longer survival for patients with melanoma, lung, or kidney cancers. Another breakthrough is CAR‑T cell therapy, a personalized treatment where a patient’s T‑cells are genetically engineered to target specific cancer markers. This approach requires sophisticated lab work, but the payoff can be dramatic, especially for certain blood cancers where remission rates have surged. Then there’s vaccine therapy, vaccines designed to teach the immune system to recognize tumor‑associated antigens. Unlike traditional vaccines that prevent infection, these aim to treat existing disease by prompting a targeted immune response. Together, these three sub‑types illustrate how immunotherapy encompasses checkpoint inhibition, cellular engineering, and antigen‑specific vaccination, each influencing patient outcomes in its own way.
Why does this matter for you? If you or a loved one are navigating a cancer diagnosis, knowing the differences can shape treatment discussions with doctors. Checkpoint inhibitors are often given as pills or infusions and may cause immune‑related side effects like skin rash or colitis. CAR‑T therapy requires an upfront cell‑collection procedure, a waiting period for lab modification, and close monitoring for cytokine release syndrome. Vaccine therapy is still emerging, usually offered within clinical trials, and focuses on preventing relapse after primary treatment. Understanding these attributes—delivery method, side‑effect profile, and target disease—helps you weigh options and ask the right questions: Which approach aligns with the cancer type? What are the chances of lasting remission? How does each option fit into the overall care plan? By connecting the dots between the central concept of immunotherapy and its major sub‑entities, you’re better equipped to navigate the rapidly evolving landscape of cancer care.
Below you’ll find a hand‑picked collection of articles that dive deeper into each of these topics. From practical guides on how checkpoint inhibitors work to real‑world stories about CAR‑T successes, the posts are organized to give you clear, actionable insights. Whether you’re starting to explore treatment options or you’re already on a specific therapy, the resources here aim to answer the most pressing questions and help you stay ahead of the latest developments in immunotherapy.