
Does Your Body Ever Fully Recover from Chemotherapy?
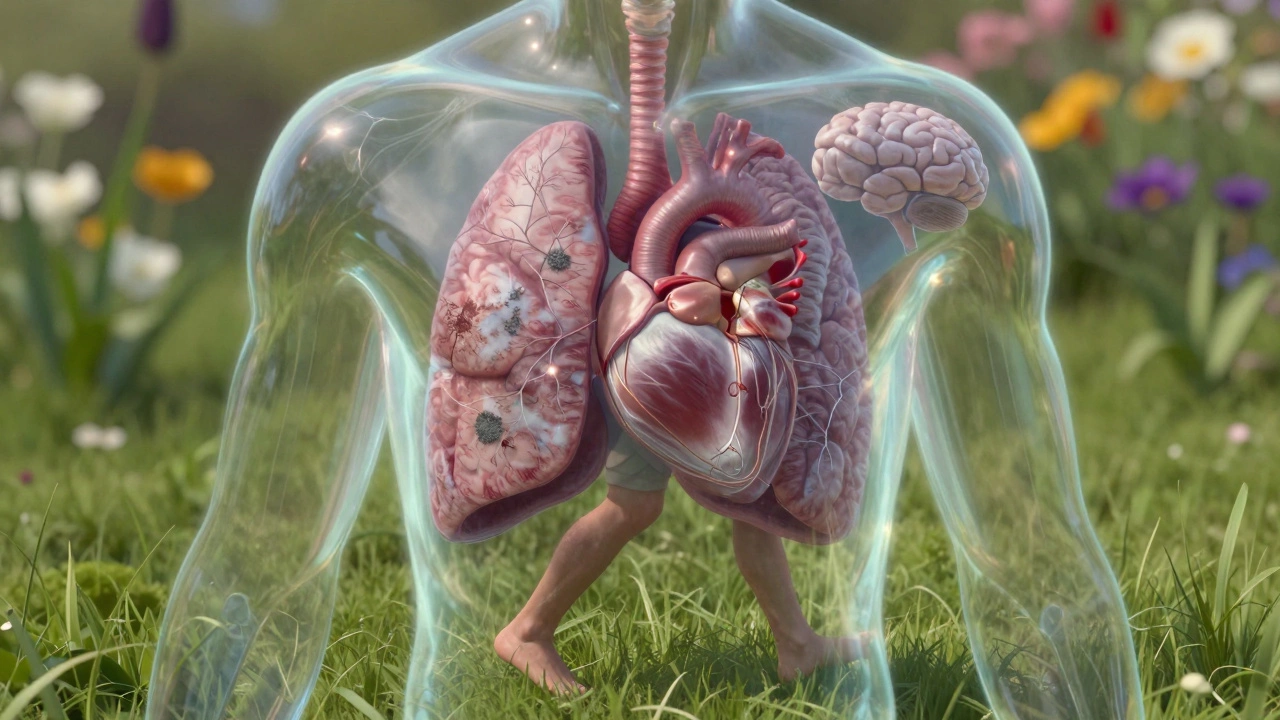
When someone finishes chemotherapy, many assume the hardest part is over. But for a lot of people, the real question isn’t whether the cancer is gone-it’s whether their body will ever feel like it did before. Chemotherapy doesn’t just attack cancer cells. It hits everything in its path: hair follicles, gut lining, bone marrow, nerves, even the heart. The damage isn’t always visible, and it doesn’t vanish the day your last IV drip ends.
What Recovery Actually Looks Like
Recovery from chemotherapy isn’t a single event. It’s a patchwork of healing, setbacks, and new normals. Some people bounce back in weeks. Others live with changes for years-or for life. The truth? There’s no universal timeline. Your body’s response depends on the type of chemo, how long you were on it, your age, your overall health before treatment, and even your genetics.
Think of it like this: if chemotherapy is a sledgehammer to your biology, recovery is the slow repair job that follows. Some parts heal completely. Others don’t. And some never get fixed-they just learn to work differently.
Common Short-Term Side Effects That Fade
Most people expect nausea, fatigue, and hair loss. And yes, those usually go away. Hair typically starts growing back within 3 to 6 months. Nausea fades as the drugs leave your system. Fatigue improves over weeks to months, though some people report low energy for over a year.
One study tracking 1,200 cancer survivors in the UK found that 72% reported significant improvement in fatigue within 12 months after finishing chemo. But 28% still felt tired at the 2-year mark. That’s not rare. It’s normal.
The Hidden Long-Term Damage
Beneath the surface, chemotherapy can leave behind quieter, longer-lasting wounds. These aren’t talked about as much-but they’re just as real.
- Chemotherapy-induced peripheral neuropathy (CIPN): Numbness, tingling, or pain in hands and feet. For some, this fades. For others, it lingers. A 2023 study in The Lancet Oncology found that 30% of patients still had moderate to severe nerve damage 5 years after treatment.
- Heart damage: Drugs like doxorubicin can weaken the heart muscle. Even if you feel fine, your heart may not be working at 100%. Cardiac monitoring after chemo isn’t routine-but it should be for high-risk cases.
- Lung scarring: Bleomycin and other agents can cause fibrosis. You might not notice until you can’t climb stairs without gasping.
- Fertility issues: Chemo can permanently damage ovaries or sperm production. Freezing eggs or sperm before treatment helps, but it’s not a guarantee.
- Cognitive changes (“chemo brain”): Memory lapses, trouble focusing, mental fog. Brain scans show real structural changes in some survivors. A 2022 study from University College London found that 40% of breast cancer survivors still had measurable cognitive decline 4 years after chemo.
Can Your Body Fully Recover?
The short answer: sometimes, but not always. And “fully” depends on what you mean.
If “fully” means going back to how you were before diagnosis-no fatigue, no tingling, no brain fog, no anxiety about relapse-then for many, the answer is no. That version of you is gone. But that doesn’t mean you can’t build something better.
Recovery isn’t about returning to the past. It’s about adapting to a new baseline. Many people find their new normal is strong, even vibrant. They move differently, eat differently, rest differently. And they’re grateful for it.
Take Sarah, a 52-year-old teacher from Brighton. She finished chemo for stage III breast cancer in 2021. Her hair grew back, her energy returned, and she went back to work. But she still gets numbness in her fingers. Her heart rate doesn’t spike like it used to. She can’t run anymore. But she hikes. She meditates. She sleeps 8 hours a night. She calls it “a different kind of health.”
What Helps Recovery the Most
Science shows that recovery isn’t just about time-it’s about action.
- Movement matters: Even light walking 30 minutes a day improves circulation, reduces fatigue, and helps nerve repair. A 2024 meta-analysis in the British Journal of Cancer found that survivors who exercised regularly had 40% less long-term neuropathy.
- Nutrition rebuilds: Chemo strips your gut of good bacteria. Probiotics, fiber, and lean protein help restore your microbiome. Zinc and vitamin B12 are critical for nerve repair. Many survivors benefit from working with a cancer nutritionist.
- Sleep heals: Deep sleep is when your body repairs tissues and clears brain toxins. Poor sleep after chemo doubles the risk of ongoing cognitive issues.
- Mental health isn’t optional: Anxiety and depression slow physical healing. Therapy, support groups, mindfulness-these aren’t luxuries. They’re part of the treatment plan.

What to Watch Out For
Some symptoms are normal. Others aren’t. Here’s what to track:
- Is your fatigue getting worse, not better?
- Do you have new numbness, weakness, or pain?
- Are you short of breath during light activity?
- Is your memory getting worse, not better?
- Are you having heart palpitations or chest tightness?
If any of these are new or worsening, talk to your oncologist. Don’t assume it’s just “part of recovery.” Some damage can be slowed-or even reversed-if caught early.
It’s Not Just Physical
Recovery isn’t just about cells and organs. It’s about identity. Many people feel like strangers in their own bodies. They grieve the version of themselves that existed before cancer. That grief doesn’t have a timeline. It doesn’t disappear with a clean scan.
And that’s okay. Healing isn’t linear. Some days you feel strong. Other days, even getting out of bed feels like a victory. Both are part of the process.
The goal isn’t to return to who you were. It’s to become someone who’s been through hell-and still chose to keep moving.
Final Thought: Recovery Is a Journey, Not a Finish Line
There’s no official checklist for “fully recovered.” No blood test, no scan, no doctor’s note that says you’re back to normal. Because “normal” changed.
What you can do: give yourself grace. Track your progress-not against who you were, but against where you are today. Celebrate small wins. Ask for help. And remember: your body doesn’t have to be perfect to be powerful.
Many people do live full, active, meaningful lives after chemotherapy. Not because they’re cured of every side effect-but because they learned to live with them, adapt to them, and sometimes, even thrive because of them.
Can chemotherapy cause permanent damage?
Yes, some chemotherapy drugs can cause permanent changes. Nerve damage (neuropathy), heart muscle weakening, lung scarring, and fertility loss are examples. The risk depends on the drug, dose, and individual factors. Not everyone gets permanent damage-but it’s common enough that long-term follow-up care is recommended.
How long does it take to recover from chemo side effects?
It varies. Nausea and fatigue often improve within 3 to 6 months. Hair regrowth usually starts in 3 months. But nerve damage, cognitive issues, and heart changes can take years-or may not fully resolve. A 2024 UK study found that 1 in 3 survivors still had noticeable side effects 5 years after treatment.
Does exercise help recovery after chemotherapy?
Yes, strongly. Regular movement-even walking-improves energy, reduces nerve pain, supports heart health, and helps with mental well-being. A 2024 meta-analysis showed that survivors who exercised at least 3 times a week had 40% less long-term neuropathy and faster cognitive recovery.
Can chemo brain be reversed?
It can improve, but not always completely. Cognitive therapy, sleep hygiene, physical activity, and managing stress can help the brain rewire. Some people regain full function. Others learn to work around memory gaps. Tools like calendars, reminders, and routine help manage ongoing symptoms.
Should I get regular check-ups after finishing chemo?
Absolutely. Follow-up care isn’t just about checking for cancer recurrence. It’s also about catching late effects early. Heart function, lung health, nerve function, and hormone levels should be monitored. Ask your oncologist for a survivorship care plan. Most hospitals offer them.

Arnav Singh
I am a health expert with a focus on medicine-related topics in India. My work involves researching and writing articles that aim to inform and educate readers about health and wellness practices. I enjoy exploring the intersections of traditional and modern medicine and how they impact healthcare in the Indian context. Writing for various health magazines and platforms allows me to share my insights with a wider audience.
About
Medical Resource Center India is a comprehensive online platform dedicated to providing reliable health information and medical resources in India. Explore a wide range of articles, tips, and advice on medicine, healthcare services, and wellness. Stay informed about the latest developments in Indian medicine and access valuable insights into maintaining a healthy lifestyle. Discover expert guidance and health solutions tailored for every Indian citizen. Your go-to destination for authoritative medical knowledge in India.






