Life Expectancy Stage 4 Cancer
When talking about life expectancy stage 4 cancer, the average time an adult lives after a stage 4 diagnosis, based on medical data and personal factors. Also known as stage 4 cancer lifespan, it helps patients, families, and doctors set realistic expectations and plan care.
Key concepts
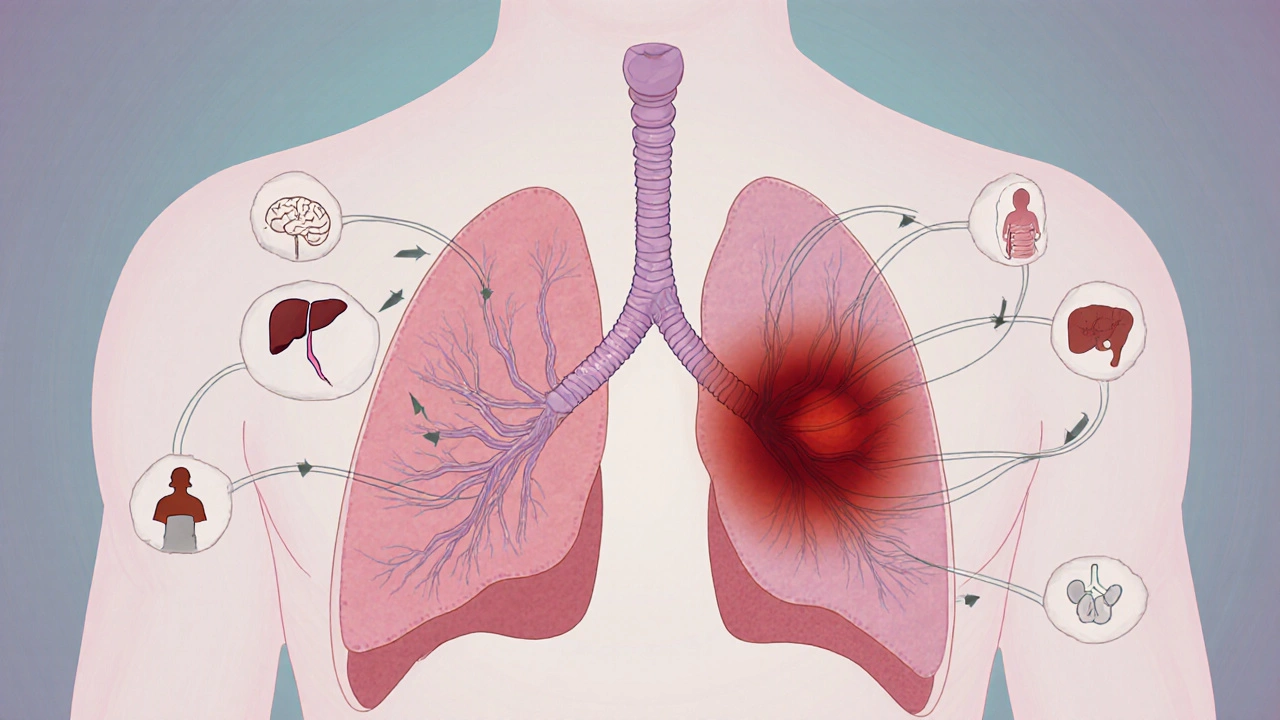
Stage 4 cancer, the most advanced cancer stage where the disease has spread beyond its original site is the starting point for any discussion about life expectancy. Once cancer reaches this point, the body faces multiple challenges: larger tumor burden, organ dysfunction, and weakened immunity. These challenges shape the average survival window, but they don’t lock everyone into the same timeline. For example, a patient with isolated lung metastases may live longer than someone whose cancer has invaded the liver and brain simultaneously.
Terminal cancer, cancer that is expected to lead to death within a short period, typically months often gets mixed up with stage 4 disease. The two are related but not identical. A stage 4 diagnosis can be managed with aggressive treatment, clinical trials, or targeted therapies that extend life beyond the “terminal” label. Conversely, some stage 4 cases are already terminal because the cancer no longer responds to any proven treatment. Understanding this nuance prevents unnecessary panic and guides better decision‑making.
Cancer survival rates, statistical measures that show the percentage of patients alive after a set number of years post‑diagnosis provide a factual backbone for life‑expectancy estimates. Worldwide data from 2020‑2024 shows that the five‑year survival for stage 4 lung cancer hovers around 7 %, while stage 4 breast cancer reaches roughly 27 % when HER2‑targeted drugs are used. These numbers are averages; individual outcomes can be better or worse depending on age, overall health, and specific tumor genetics.
Palliative care, a multidisciplinary approach that relieves symptoms and improves quality of life for serious illness becomes a central piece of the puzzle once curative options run out. It isn’t just end‑of‑life hospice; it includes pain management, nutritional support, mental‑health counseling, and assistance with daily activities. Studies show patients who receive early palliative care often live longer than those who wait until the final weeks. The care team works side‑by‑side with oncologists to balance treatment benefits against side‑effects.
Several personal factors tweak the baseline life‑expectancy figure. Age matters—older adults generally have shorter horizons because of reduced organ reserve. The specific organs involved also count; brain metastases carry a poorer prognosis than bone lesions. Genetic mutations (like EGFR or KRAS) can open doors to targeted drugs that dramatically extend survival. Lifestyle choices such as smoking cessation, balanced nutrition, and moderate exercise have been linked to modest gains in lifespan, even at stage 4.
Practical steps help patients and families navigate this uncertain terrain. First, request a detailed prognosis that breaks down median survival, best‑case, and worst‑case scenarios. Second, discuss all available treatment lines, including clinical trials, immunotherapy, and supportive therapies. Third, set up a solid support network—family, friends, support groups, and a dedicated palliative team. Finally, establish clear goals: what symptoms are unacceptable, which activities remain non‑negotiable, and how much treatment burden one is willing to endure.
Below you’ll find a curated collection of articles that dive deeper into each of these topics. From the science behind survival statistics to real‑world tips on managing symptoms, the posts are designed to give you actionable insight and a clearer picture of what life expectancy looks like for stage 4 cancer patients.