- Home
- Orthopedics
- Effective Medications for Orthopedic Swelling: A Practical Guide
Effective Medications for Orthopedic Swelling: A Practical Guide
Orthopedic Swelling Medication Guide
Choose Your Situation
Recommended Approach
Key Considerations
Important Warning
When an injury hits a joint or bone, swelling is the body’s way of saying, “I need help right now.” But the extra fluid can lock you down, hurt your range of motion, and slow recovery. Knowing orthopedic swelling medication options helps you cut the puff and get moving again-without guessing or grabbing the first pill you see.
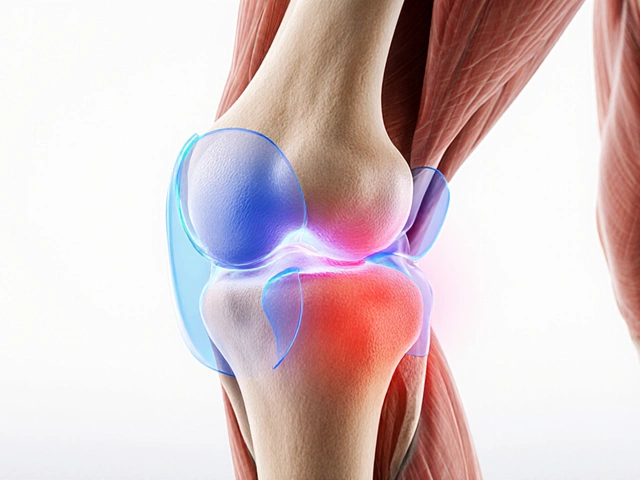
What is orthopedic swelling?
Orthopedic swelling is the accumulation of fluid, inflammatory cells, and tissue fluid around a musculoskeletal injury such as a sprain, fracture, or post‑surgical site. It’s a normal part of the healing cascade, but when it becomes excessive, pain rises and mobility drops.
The drug families that actually reduce the swelling
Not every painkiller works the same. The main drug families used by orthopedists are:
- Non‑steroidal anti‑inflammatory drugs (NSAIDs)
- Corticosteroids (oral or injectable)
- Topical anti‑inflammatories
- Acetaminophen (for pain only)
- Short‑term opioids (rarely, for severe pain)
Each class targets a different step in the inflammation pathway. Below we break down how they work, when doctors prefer them, and what you should watch out for.
NSAIDs - the frontline fighters
NSAIDs block cyclo‑oxygenase (COX) enzymes, which drive prostaglandin production-the chemicals that cause swelling and pain. They’re the go‑to for most acute orthopedic injuries because they act fast and are inexpensive.
Common oral NSAIDs you’ll see prescribed or bought over the counter include:
- Ibuprofen (200‑800mg every 6‑8hours)
- Naproxen (250‑500mg twice daily)
- Diclofenac (50‑150mg 2‑3 times a day)
These drugs start to work within 30‑60minutes, peak at about two hours, and stay active for 4‑12hours depending on the specific agent. For patients with stomach sensitivity, doctors often add a proton‑pump inhibitor (like omeprazole) to protect the lining.
Side‑effect checklist:
- Gastro‑intestinal irritation or ulcers
- Increased blood‑pressure, especially with chronic use
- Kidney function impact-avoid high doses if you have renal disease
Because they’re reversible, you can stop NSAIDs once swelling subsides (usually 5‑7days for mild injuries).
COX‑2 selective inhibitors - smoother on the stomach
For people who can’t tolerate traditional NSAIDs, COX‑2 inhibitors like Celecoxib (200mg once or twice daily) provide similar anti‑inflammatory effects with less gastric irritation. The trade‑off is a slightly higher cardiovascular risk, so they’re best for short‑term use in patients without heart disease.
Corticosteroids - the heavy‑hit option
Corticosteroids are synthetic versions of the body’s own cortisol hormone. They shut down the entire inflammatory cascade, not just prostaglandins. Orthopedic surgeons reserve them for cases where swelling is stubborn-often after surgery or in severe joint effusions.
Typical oral choices:
- Prednisone (5‑20mg daily, tapering over 1‑2weeks)
- Methylprednisolone (similar dosing schedule)
Injectable steroids (e.g., triamcinolone) are delivered directly into the joint or surrounding tissue for rapid local control. The effect can last weeks, but repeated injections increase the risk of tissue thinning and infection.
Key warnings:
- Raise blood‑sugar levels-important for diabetics
- Potential mood swings or sleep disturbance
- Long‑term use can weaken tendons and cartilage
Because of these downsides, doctors limit systemic steroids to under two weeks for most orthopedic patients.
Topical anti‑inflammatories - spot treatment
When swelling is localized (e.g., a knee sprain or ankle strain), a topical agent can hit the target without systemic exposure. The most evidence‑backed option is Topical diclofenac gel or patch, applied 3‑4times a day.
Benefits include:
- Minimal gastrointestinal side effects
- Easy to combine with oral NSAIDs if needed
- Rapid onset (15‑30minutes) for superficial tissue
Patients with sensitive skin should patch‑test first, and avoid using on broken skin.
When drug therapy isn’t enough - adjuncts that matter
Even the best medication won’t shrink swelling if you keep stressing the joint. Orthopedic care teams pair drugs with physical measures:
- Ice therapy: Apply a cold pack for 15‑20minutes every 2‑3hours during the first 48hours. Cold causes vasoconstriction, which reduces fluid leakage.
- Compression: Elastic wraps keep the tissue snug, limiting fluid accumulation.
- Elevation: Keeping the limb above heart level encourages venous return.
- Physical therapy: Guided range‑of‑motion exercises prevent stiffness and promote lymphatic drainage.
These non‑drug tools work synergistically with medication, often allowing you to use a lower drug dose.

Choosing the right plan - a quick decision matrix
| Drug class | Typical agents | Onset | Typical duration | Key side effects |
|---|---|---|---|---|
| NSAIDs (non‑selective) | Ibuprofen, Naproxen, Diclofenac | 30‑60 min | 4‑12 hrs | GI irritation, ↑BP, renal impact |
| COX‑2 selective | Celecoxib | 1‑2 hrs | 12‑24 hrs | Cardiovascular risk |
| Corticosteroids (oral) | Prednisone, Methylprednisolone | 2‑4 hrs | Days‑weeks (tapered) | Hyperglycemia, mood changes, tissue thinning |
| Injectable steroids | Triamcinolone, Methylprednisolone acetate | Immediate | Weeks | Joint infection, cartilage damage |
| Topical NSAID | Diclofenac gel/patch | 15‑30 min | 4‑8 hrs | Skin irritation |
Use this matrix as a starting point. Your orthopedist will factor in your medical history, injury severity, and any allergies before locking in a regimen.
Red flags - when to seek immediate medical help
Even the best medication won’t fix a serious problem. Call your surgeon or go to the emergency department if you notice:
- Rapidly increasing swelling that spreads beyond the injury site
- Severe pain that isn’t relieved by the prescribed dose
- Fever, chills, or a foul‑smelling wound (signs of infection)
- Sudden loss of sensation or inability to move the joint
- Blood in the joint fluid after a puncture or injection
Putting it all together - a sample 5‑day plan
- Day 1‑2: Ice for 20minutes×3, compression bandage, elevation. Start Ibuprofen 400mg every 6hours with food.
- Day 3‑4: Continue ice every 4hours. Add Topical diclofenac gel 3times a day if skin tolerates.
- Day 5: If swelling is still >50% of original, discuss a short course of Prednisone 10mg daily for 5days with a taper.
- Throughout: Gentle range‑of‑motion exercises guided by a physiotherapist, focusing on pain‑free movement.
- Monitor: Record pain scores and swelling measurements. If pain >5/10 despite meds, call your surgeon.
This schedule balances drug action, side‑effect risk, and non‑pharmacologic support. Adjust based on personal response and doctor advice.
Frequently Asked Questions
Can I take NSAIDs if I have high blood pressure?
Short‑term NSAIDs can raise blood pressure a bit. If you have uncontrolled hypertension, discuss alternatives like COX‑2 inhibitors or topical agents with your doctor first.
Is it safe to combine ibuprofen with acetaminophen?
Yes, the two work via different pathways, so stacking them can give better pain relief without adding extra GI risk. Keep each at the recommended dose and avoid exceeding 24‑hour limits.
How long should I wait before getting a steroid injection?
Most orthopedists wait at least 2‑3weeks after surgery or a fresh fracture, unless swelling is impairing function dramatically. The waiting period lets the initial healing phase settle.
Are there natural alternatives to reduce swelling?
Herbal anti‑inflammatories like curcumin or bromelain can help mildly, but they’re not as potent as NSAIDs. They’re useful as adjuncts once the acute phase passes.
When should I switch from oral NSAIDs to a topical gel?
If you develop stomach upset, or if swelling stays localized to one area, moving to a topical diclofenac gel can maintain anti‑inflammatory effect while sparing your gut.

Arnav Singh
I am a health expert with a focus on medicine-related topics in India. My work involves researching and writing articles that aim to inform and educate readers about health and wellness practices. I enjoy exploring the intersections of traditional and modern medicine and how they impact healthcare in the Indian context. Writing for various health magazines and platforms allows me to share my insights with a wider audience.
Popular Articles
About
Medical Resource Center India is a comprehensive online platform dedicated to providing reliable health information and medical resources in India. Explore a wide range of articles, tips, and advice on medicine, healthcare services, and wellness. Stay informed about the latest developments in Indian medicine and access valuable insights into maintaining a healthy lifestyle. Discover expert guidance and health solutions tailored for every Indian citizen. Your go-to destination for authoritative medical knowledge in India.